An X-ray of the Greek Health System during the pandemic shows that many of the COVID-19 ICUs across the country are understaffed and demonstrates a correlation between deaths and hospital occupancy during the “second wave”. The lesson of Northern Greece for Attica.
Pandemic Death Toll Seems to Be Higher Than Reported
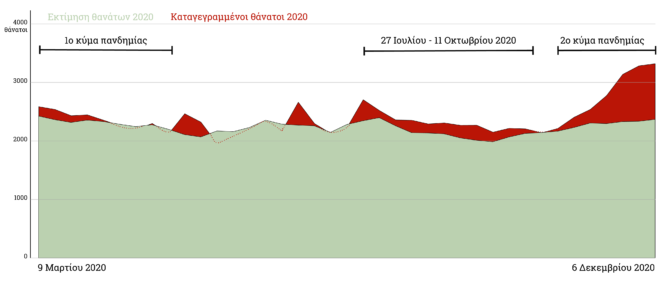
Increase in excess mortality in Greece, where a mere 43% of excess deaths were confirmed to be associated with COVID-19
What does “95% efficacy” mean?

What do the vaccine efficacy rates indicate for our everyday lives and what do we expect from the vaccination?
At the time of writing, on the morning of Tuesday, March 9, 2021, the Minister of Health, Vassilis Kikilias, announced that two private clinics, LETO Hospital and Athens Medical Centre Peristeri, are voluntarily offered to the Greek National Health System for the treatment of COVID-19 cases, under the administration of the 1st and 2nd Health District respectively, starting Thursday, March 11 –one day before the one year anniversary of the first registered COVID-19 death in our country.
The private sector contribution comes almost a week after the emergency announcements, on March 3, 2021, from the Ministry of Health and the Civil Protection, during which it was disclosed that the bed occupancy in Intensive Care Units (ICU) for COVID-19 patients in Attica had already reached 90.6% –after the system “rallied” to increase both acute care beds and intensive care beds for the treatment of COVID-19 cases, in the Athens Basin in February. At that time, during the same briefing, the Minister of Health had stated: “at the rate of new admissions to our hospitals, you all realize that the health system is exceeding its limits in terms of both infrastructure and human resources”.
As for the latter, of course, the Greek Health System appears to have exceeded its limits for some time, given the understaffing of COVID ICUs, as this is highlighted in the data analysis published by the iMEdD Lab: understaffed intensive care units for patients with COVID-19 in terms of nursing personnel in all seven Health Districts across the country (excluding military hospitals), while various units, across the State, have operated with insufficient medical personnel. These conclusions emerge from the analysis of the primary data, from 51 COVID-19 ICUs in 41 hospitals throughout Greece, which the Hellenic Society of Intensive Care Medicine (HSICM) offered to the iMEdD Lab. With a recording period from January 28 to February 18, the data include the number of beds per COVID-19 ICU (504 beds in total in the 51 ICUs under study) and the corresponding numbers of healthcare personnel: a total of 454 doctors and 1,481 nurses, including all those who have been “recruited” for the intensive care of the patients –specialists and not, permanent, auxiliary and other emergency support personnel.
Understaffed intensive care units for patients with COVID-19 in terms of nursing personnel in all seven Health Districts across Greece, while various units, across the country, have operated with insufficient medical personnel.
The analysis of the sample regarding the staffing of the units was based on the unanimous decision of the Central Board of Health (KESY) for the minimum standards for the operation of intensive care units, composed as early as June 2016. Among other things, the decision states that “an ICU must have at least six beds. Hospitals with less than six beds should be encouraged to restructure the units in order to create a larger ward, with the aim of increasing efficiency. Provably, the correct number of beds, from a financial and functional point of view, but also in terms of the experience of the personnel, is eight”. The passage reminds us of what we have forgotten in times of pandemic: the concept of an “ICU bed” as an independent entity does not exist. By definition, the ICU is an organized, high standard, set of beds.
Unfortunately, we cannot know the exact –and each time updated– number of beds, nurses and doctors in COVID-19 ICUs per Health District: the competent bodies have never, to date, disclosed data on the staffing of hospitals during the pandemic, adding to the fragmentary, periodic, update regarding the existing infrastructure. Specifically, the Ministry of Health proceeded to regular briefings regarding the available and occupied beds, per Health District, for COVID-19 cases only in the period from November 13 to November 20, 2020. There has been no regular release of data since, and there has been no response to repeated requests from the iMEdD Lab to the Ministry of Health.
For these reasons, the following analyses are based on the above sample and present analogies, that is the bed-personnel ratio per ICU, which is a more reliable indicator of the “big picture” of COVID ICU staffing –which, after all, can be underrated or overrated depending on the current status. Absolute numbers should be read with extreme caution in an ever-changing situation, the data of which are not sufficiently communicated by the Authorities.
The ICUs lack nursing personnel
Four –trained in intensive and emergency medicine– nurses per ICU bed is defined as the minimum requirement for operation (KESY, 2016); but it is not met: the average ratio of nursing personnel per COVID-19 ICU bed ranges from two to three people in each Health District, with the exception of military hospitals. Of the 51 COVID-19 ICUs under study, only the 11 seem to meet the above minimum requirement for operation. “Unfortunately, it is a fact. The intensive care units lack nurses”, comments Professor Anastasia Kotanidou, President of HSICM and head of the Scientific Committee for the planning of the new ICU beds in the hospitals of the Greek Health System.
Ratio of specialized nursing personnel per COVID ICU bed
In the data provided to us by the HSICM, many units report special notes regarding the numbers of healthcare personnel included in the total recorded figures of their staff, even though these employees serve in the COVID-19 ICUs due to the current needs, without having received training in intensive care treatment (residents, those transferred from other departments, etc).
Such nursing personnel, where explicitly mentioned, is not included in the analysis of the data presented in the above graph. Having said that, it is an important fact that in the 3rd Health District (Macedonia), which was particularly affected by the pandemic during the so-called “second wave” last winter, no ICU, from those included in our sample, meets the minimum requirement for operation. At the same time, it is worth to point out that the ICUs for Children and Military Hospitals operate with nursing personnel above the minimum requirement. The General Hospital of Thessaloniki “Agios Pavlos” and the General Hospital of Mytilene, which seem to more than meet the needs for nursing personnel, report that this includes nurses who work “in both ICUs, general and COVID” –on “a rota”, as is noted in “Agios Pavlos”.
The median ratio of nursing personnel per COVID-19 ICU bed ranges from two to three people in each Health District. Four nurses per ICU bed is defined as the minimum requirement for operation.
However, the picture of understaffing does not change, even when we include to our analysis the total nursing personnel, with or without specialization in intensive care, corresponding to the COVID ICUs, according to the data –the median ratio of nursing personnel per ICU bed continues to amount, in each Health District, from two to three people, while 13 out of the 51 ICUs under study seem to operate with the minimum required personnel or above.
Ratio of nursing personnel per COVID ICU bed (non-specialized personnel included)
Shortages or marginal medical personnel in several ICUs
Even if we include in our analyses the total amount of the medical personnel who are proclaimed to have been “recruited” and employed in the COVID ICUs (apart from the permanent and auxiliary intensive care doctors, seconded employees, specialty doctors, residents, those transferred from other departments and anesthesiologists) many ICUs across the State operate well below an ideal ratio of “1 to 1” (one doctor per bed) –with the corresponding median ratio, at Health District level, not ensuing in half of the districts.
Ratio of ICU doctors-beds for patients with COVID-19
According to the unanimous decision of KESY (2016), at least six doctors, with the required specialization for the practice of intensive care, for eight ICU beds are “necessary for the safe and unobstructed operation of the unit”. For ICUs larger than eight beds, the proportion of the number of doctors should be one doctor for every three extra beds. “In ICUs with four to six beds, the medical personnel cannot be comprised by less than six people, in order to cover on call duties” the same decision states.
Given the different minimum requirement for operation, depending on the beds available, we calculated whether the minimum requirement is met for each COVID-19 ICU for which we have been provided with data. Again, in our analysis, considering the special conditions in times of pandemic, we initially took into account the total number of medical personnel that reportedly corresponds to each unit –regardless of the individual working situation and any professionals who are not specialized in intensive care.
Several ICUs have been inadequately or marginally staffed in terms of medical personnel –especially out of the Health Districts impacted by the Athens Basin’s resources.
Even so, it is clear that several units (11 out of 40) have been inadequately or marginally staffed –especially out of the 1st and 2nd Health Districts, that is out of the districts impacted by the Athens Basin’s resources. It is noted that, in the context of this particular analysis, eight ICUs, which reportedly contain less than four beds, that is less than the exceptionally proposed minimum infrastructure (KESY, 2016), were excluded from the sample. These are the ICUs in the General Hospitals of Mytilene, Kozani (Mamatseio), Rethymno, Agios Nikolaos, the Children’s ICUs in Ippokrateio of Thessaloniki and the university General Hospitals of Patras and Heraklion as well as the ICU in the 251 Air Force General Hospital.
Staffing of COVID-19 ICU beds with medical personnel (non-specialized or emergency support personnel included)
“In order for this infrastructure to be able to function, it requires very specialized personnel. If you take any doctor and put them in an ICU, it is as if you take me, put me on a plane and tell me ‘go ahead, fly it now’”, says Nikos Kapravelos, Department Manager of the Intensive Care Unit and Coordinating Director of the 2nd ICU at Papanikolaou Hospital in Thessaloniki, commenting on the question of reinforcing COVID ICUs with personnel from other specialties or trainees. He recalls the experience of the period from November 1 to January 15, when the 2nd ICU at Papanikolaou Hospital was among those which carried the weight of the severe “second wave” that struck Northern Greece, and he continues, regarding the increased demands due to the pandemic: “The COVID ICU needs one and a half times more personnel (editor’s note: than the minimum required under normal circumstances): you need twice the amount of personnel in order to enter the wards. With the mask we wear, which is highly protective, along with the face shield we have, with all this equipment, you cannot breathe properly –(editor’s note: the employees) cannot work for more than three hours the most. When you see them coming out of the wards, you feel sorry for them. We had such images, but you will see them in Athens now, the pressure is terrible”.
In the COVID ICU , you need twice the amount of personnel in order to enter the wards. With all this equipment, you cannot breathe properly. When you see them coming out of the wards, you feel sorry for them.
Nikos Kapravelos, Department Manager of the ICU and Coordinating Director of the 2nd ICU at Papanikolaou Hospital in Thessaloniki
Looking at the fixed needs that exist due to the pandemic, Nikos Kapravelos also comments on the issue of filling up organic positions of doctors and nurses: “Shortages are a chronic problem, which, however, now that things are supposed to be falling into place, must stand out in its true dimension. Yes, we have been saying that ‘we will go in, we will give our battle, we will die like heroes’ and so on, but now the needs that arise are permanent and one has to see and highlight them –the extent of understaffing is tragic” .
Indeed, when the data analysis is adjusted to exclude staff from other specialties, trainees, auxiliary personnel, or transferred, or seconded staff, half of the units (19 out of 40) in all Health Districts across the country are in the “red zone”.
Staffing of COVID-19 ICU beds with permanent medical personnel
ICU on standby means adequate medical and nursing personnel, who must be specialized in intensive care. It also means physiotherapists, ward assistants, paramedics.
Professor Anastasia Kotanidou, President of HSICM and head of the Scientific Committee for the planning of the new ICU beds in the hospitals of the Greek Health System
I am absolutely satisfied with the readiness demonstrated by the ICU personnel. In the months of January and February, we had 1,227 admissions to ICUs nationwide. In these admissions, the mortality rate was around 35%. There is no system that can withstand such pressure –not even in highly organized Germany.
Professor Anastasia Kotanidou, President of HSICM and head of the Scientific Committee for the planning of the new ICU beds in the hospitals of the Greek Health System
“ICUs on standby”, although understaffed
“Once we have secured beds, monitors and respirators (and spare), ICU on standby means adequate medical personnel, who must be specialized in intensive care. It means adequate nursing personnel, who must also be specialized in intensive care. It also means physiotherapists, ward assistants, paramedics –all of them are the personnel that a unit needs to be on standby and operational”, explains Professor Anastasia Kotanidou, President of HSICM and head of the Scientific Committee for the planning of the new ICU beds in the hospitals of the Greek Health System.
Then, Anastasia Kotanidou clarifies the importance of the multifunctional ICU in general: “In Greece, there is confusion regarding some basic things: there are ICU beds which are multifunctional ICU beds. In order for a unit to be called multifunctional, it must be supported by many departments within the hospital and be supporting many departments: that is, if it receives a polytraumatized patient, it must have a neurosurgeon, thoracic surgeon, cardiovascular surgeon, orthopedic, which means that the hospital where the ICU belongs must have the corresponding specialties. Imagine that, in some islands, there are very small hospitals with one internist and a pediatrician, and all the other specialties are missing. These small islands do not have the capacity for multifunctional ICU beds. They have the capacity for some beds, possibly, under certain conditions, of intermediate care (IMCU), capable of stabilizing the patient, so that they can be transferred to a multifunctional ICU. Similar problems also exist in some areas in mainland Greece. The hospital of Kilkis, for example, has neither an IMCU nor an ICU”.
When asked whether, until now, she is satisfied with the readiness of the system for the treatment of COVID-19 cases in hospitals, in Attica or nationwide, Anastasia Kotanidou answers to the iMEdD Lab: “I am absolutely satisfied with the readiness demonstrated by the ICU personnel. In the months of January and February, we had 1,227 admissions to ICUs nationwide. In these admissions, the mortality rate was around 35%. There is no system that can withstand such pressure –not even in highly organized Germany. We managed to treat 1,227 patients in the ICUs within two months and not only did we endure, but we also had a fatality rate of 35%”.
She claims that the understaffing of the ICUs “in terms of dealing with the pandemic at the moment means nothing, thanks to the earnest efforts of our colleagues. Colleagues in understaffed hospitals go out of their way, so that the level of care to be equivalent to that of central hospitals”. Then, speaking specifically about the latter, the large hospitals which, in general, seem to cover their staffing needs, Kotanidou points out: “Some hospitals, such as Attiko, Evaggelismos, partly the General Hospital of Athens, the General Hospital of Piraeus, are hospitals that accept whichever case is more severe. That is, in these hospitals you may see extracorporeal oxygenation (ECMO). You will not see it in Giannitsa, Serres or Drama. These cases require two to three doctors and two nurses stand by, 24 hours a day. COVID patients primarily may need ECMO. The respiratory failure that the disease can cause is very severe and, when we are not able to oxygenate them, we proceed to extracorporeal oxygenation. In regional hospitals, such as Drama or Kilkis, they do not have the opportunity to do so because they do not have cardiac surgery departments. In these cases, the patient is transferred to a central hospital, which has the ability to use ECMO” –in a central hospital in Alexandroupolis or Thessaloniki, which last winter, due to pressure, “had to turn operating theaters into ICUs in no time, and any space that had an oxygen supply also had to be converted into an ICU”.
Hospital occupancy and fatalities
As it is known, until today, Northern Greece has paid the heaviest toll in human lives from the pandemic. In fact, as the iMEdD Lab has showcased, Drama, Pella, Pieria, Kilkis, Serres, Grevena, Imathia, Kavala, Thessaloniki and Xanthi are the ten regional units of the country that, in proportion to their population, have the most victims to mourn.
Mortality and hospital occupancy during the second “wave” of the pandemic in Greece
Μost of the deaths in Northern Greece, at 75%, occurred outside the ICU. The patients were going to the hospital very late, they were in a very serious condition and did not manage to make it to the unit.
Professor Anastasia Kotanidou, President of HSICM and head of the Scientific Committee for the planning of the new ICU beds in the hospitals of the Greek Health System
These people who came in, were very old and this is the variant between the second and the third ‘wave’: the patients were very old, which means that you couldn’t afford a single hour to support the patient, to find an empty intensive care bed –old age, rapid death.
Nikos Kapravelos, Department Manager of the ICU and Coordinating Director of the 2nd ICU at Papanikolaou Hospital in Thessaloniki
The analysis of the information of the recent past, using, on the one hand, the latest data published by the Ministry of Health (on November 20) regarding the available and occupied beds in ICUs and in total per Health District, and, on the other hand, the geographical distribution of losses, from the beginning of the pandemic, which the iMEdD Lab published in mid-December, results in a positive correlation between deaths and hospital occupancy: in general, it appears that the higher the bed occupancy, the higher the mortality from the pandemic (deaths/100,000 local population) in each area. Unfortunately, the leading examples are the 3rd and 4th Health Districts (Macedonia and Macedonia & Thrace, respectively), where both hospital occupancy and mortality have “hit red”, despite the, compared to other areas, higher availability of beds which, as it turned out, wasn’t enough.
“This is internationally known (remember what happened in Italy): the more complete a department is, the higher the fatality rate. That is, the higher the workload, the higher the fatality rate”, confirms Anastasia Kotanidou, maintaining that the understaffing of the ICUs is not related to the fatalities, thanks to the employees who go out of their way.
She also recalls that “most of the deaths in Northern Greece, at 75%, occurred outside the ICU” and explains that this happened, “because the patients were going to the hospital very late, they were in a very serious condition and did not manage to make it to the unit”. Speaking about the correlation between deaths and hospital occupancy of acute care beds, Kotanidou states that “if in a hospital, one nurse cares for 70 patients, it is completely normal to not be able to provide the care that would be provided to 20”. And then she explains: “The conditions in the ICU are different from the medical floor. In the ICU, even in understaffed conditions, a nurse can care for up to three patients. On the floor, a nurse may have 50, 60 or even 70 patients, as the case may be. The ratio is completely different. This does not mean that the ICUs can operate to their full capacity when they are systematically understaffed. The ICU cases are very serious, the demands are very high and the limits of the personnel’s endurance are not inexhaustible”.
The lesson of Northern Greece for Attica
Nikos Kapravelos seems to confirm the above, recalling the data from Papanikolaou Hospital in Thessaloniki: “In 2020 we had approximately 1,700 admissions of COVID-19 patients (in total, both in the ICU and on the floor). In the ICUs, we had around 240 patients and 60-70 deaths. From the others, we had about 200 deaths”. The severity of the “wave”, that is the large number of serious cases, their age and the lack of ICU beds, Kapravelos summarizes, were the causes of the losses on the floor, outside the ICU.
He explains: “These people who came in, were very old and this is the variant between the second and the third ‘wave’: the patients were very old, which means that you couldn’t afford a single hour to support the patient, to find an empty intensive care bed –old age, rapid death. The deterioration was very rapid. Obviously, there was a lack in ICUs because the needs were far greater than the capabilities we had. This is well-known. Therefore, many were not given the opportunity to go through an ICU. Also, many left the ICU and died in the department: the cases were so serious and such was the pressure put on us for someone who was a little better to leave (editor’s note: the ICU)… However, the conditions were not such (editor’s note: to move to an acute care bed). They had to go to an IMCU, which does not exist in Papanikolaou. It helped us a lot that some of these cases were diverted to a private center that, after a deal with the state, was taking such cases for intermediate care. And many people were saved that way”.
Now that Attica can rely on the course of vaccinations and the younger average age of the patients, Kapravelos also conveys the following lesson, from Northern Greece to the capital: “to not come to the nightmare of seeking for ICU beds and be unable to find them, to pay attention to exactly this circulation, to not rush to discharge patients (editor’s note: from the ICU) and then lose them in the department, to try to exploit the ICUs of the private sector. Our experience tells us that it needs a lot of attention: it is not only the ICU, it is also the management after the intensive care unit. “These patients stay for a long time (editor’s note: in the ICU) and they may rush, under pressure, to discharge patients, which will be unfair losses”.
Translation: Evita Lykou